Beyond Weight: Let's break the stigma of obesity
March 13, 2025

Obesity is a health condition that goes beyond body weight. Despite scientific advances, a mistaken perception persists, reducing it to a matter of willpower or personal discipline. This perception contributes to significant stigma, affecting the quality of life of individuals living with obesity and making it difficult to access appropriate treatments (Rubino et al., 2020).
🔬 What Is Obesity Stigma?
Obesity stigma refers to the prejudices and discrimination faced by individuals with this condition in different areas of society. This phenomenon is based on the erroneous belief that body weight is entirely controllable and that people with obesity have failed in their self-care. However, science has shown that obesity is a multifactorial condition influenced by genetic, metabolic, environmental, and socioeconomic factors (Sánchez-Carracedo, 2022).
One of the areas where stigma is most evident is in healthcare. Studies have shown that healthcare professionals may exhibit implicit biases against patients with obesity, leading to delayed diagnoses and inadequate treatments (Nutter et al., 2023). This results in lower healthcare access rates and poorer quality of care, which can negatively affect the progression of obesity-related diseases.
Additionally, a new classification proposal distinguishes between preclinical obesity (excess adiposity without evident organ dysfunction) and clinical obesity (when adiposity causes alterations in organs and tissues), reinforcing the idea that obesity is not just about weight but a disease with systemic impacts (The Lancet Diabetes & Endocrinology, 2025). The commission also emphasizes that obesity should not be assessed solely through BMI but also with other measures such as waist circumference or waist-to-height ratio, as BMI alone does not reflect the complexity of the condition (Rubino et al., 2025).
🧬 Factors Contributing to Obesity: A Comprehensive Approach
Contrary to popular belief, obesity is not simply the result of an unbalanced diet or lack of physical activity. It is a condition with a multifactorial origin, where genetic, metabolic, environmental, and socioeconomic factors interact, each playing a crucial role in its development (Chiurazzi et al., 2020).
1. Genetic Factors: Inherited Predisposition
It is estimated that 40% to 70% of obesity risk is determined by genetics. Mutations in genes such as MC4R, POMC, and FTO can influence appetite regulation, fat storage, and metabolic efficiency (Chiurazzi et al., 2020). Additionally, epigenetic factors can modify the expression of these genes, promoting obesity in certain environments and lifestyles.
🔬 Key Genetic Mechanisms:
Hunger and satiety regulation: Leptin function alterations can lead to increased appetite.
Basal metabolism: Some genetic variations affect the resting metabolic rate.
Food preferences: Studies have shown that certain genes can influence a preference for foods rich in fats and sugars.
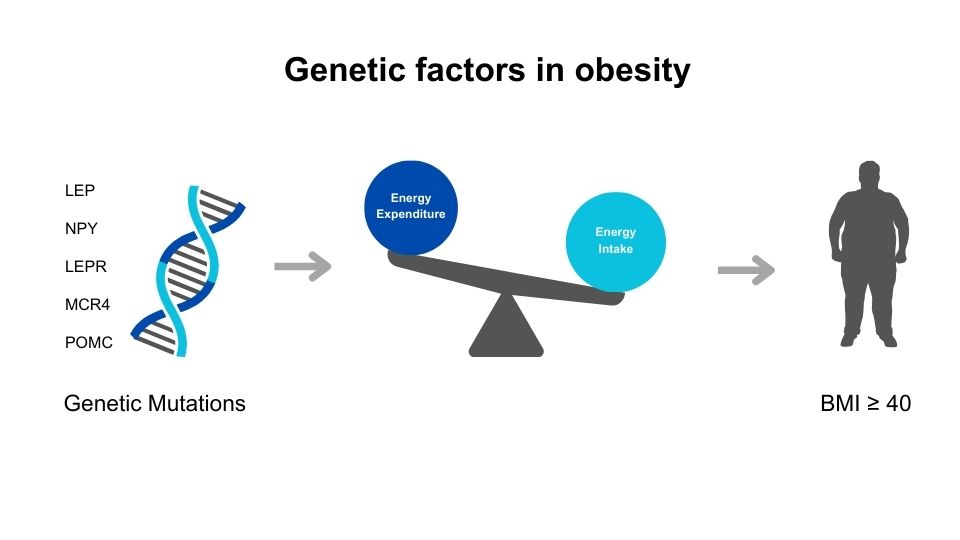
Figure 1. Genetic factors in obesity: Genes involved in appetite regulation and metabolism. Self-created image based on Chiurazzi et al. (2020). International Journal of Molecular Sciences. Source: https://doi.org/10.3390/ijms21239035, under CC BY 4.0 license.
💡 Key Fact: While genetics play a crucial role, they do not determine fate. Epigenetic and environmental factors can modulate their effects.
2. Obesogenic Environment: A System That Promotes Excess Weight
The term "obesogenic environment" refers to environmental conditions that facilitate weight gain and make adopting a healthy lifestyle more challenging.
The "obesogenic environment" promotes weight gain and hinders the adoption of a healthy lifestyle. Uncontrolled urbanization and exposure to ultra-processed diets have created an environment where healthy choices are not always accessible (Wang et al., 2019; Roe et al., 2020). Additionally, the lack of adequate spaces for physical activity and increasing sedentary lifestyles have worsened the problem (The Lancet Diabetes & Endocrinology, 2025).
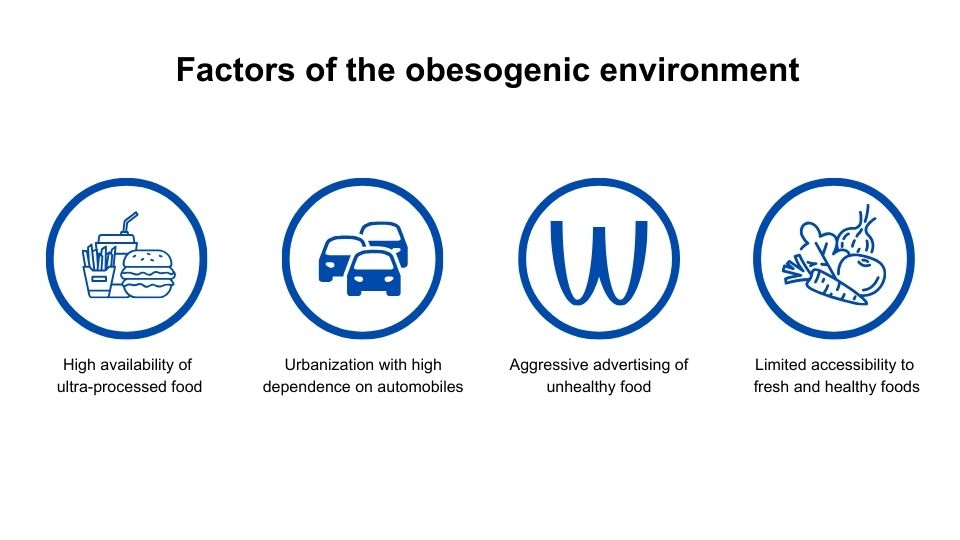
Figure 2. Obesogenic environment factors. Self-created image.
Some examples include:
🍔 Availability of ultra-processed foods: In many cities, ultra-processed and low-nutritional-value foods are more accessible and affordable than healthier options.
🚶♀️ Sedentary lifestyles: Technology and urbanization have reduced daily physical activity (office jobs, motorized transport, long work hours).
🏙️ Limited access to healthy food: In many urban and rural areas, fresh fruits and vegetables can be expensive or difficult to find, forcing reliance on less nutritious options.
📺 Advertising and consumer culture: Constant exposure to fast food and sugary drink advertisements influences food choices, especially among children and adolescents.
💡 Key Fact: A healthy environment can prevent obesity even in people with a genetic predisposition, highlighting the importance of public policies in nutrition and health.
3. Socioeconomic Factors: The Impact of Stress and Inequality
Economic and job insecurity can increase cortisol production, a hormone that promotes abdominal fat storage. Additionally, stress can alter the function of leptin and ghrelin, hormones that regulate hunger and satiety (Rubino et al., 2020). Socioeconomic factors have also been shown to affect access to medical care and effective treatments (The Lancet Diabetes & Endocrinology, 2025).
🔄 Chronic Stress and Hormonal Dysregulation:
Prolonged stress exposure (job instability, financial insecurity, discrimination) increases cortisol production, a hormone that promotes abdominal fat accumulation.
Stress can also alter leptin and ghrelin function, increasing the tendency to overeat (Rubino et al., 2020).
🚧 Lack of Access to Healthy Opportunities:
In low-income communities, fast food is cheaper than nutritious foods.
The lack of safe spaces for physical activity limits opportunities to maintain an active lifestyle.
💡 Key Fact: Obesity is not just an individual issue but a reflection of social inequalities. To reduce its prevalence, it is crucial to address economic and environmental barriers that hinder healthy eating and exercise.
4. Limitations to Physical Activity: Exercise for Whom?
Despite the well-documented benefits of exercise, not everyone has the same opportunities to be active. The lack of access to adequate spaces is a key factor in the development of obesity (Brito et al., 2021; Roe et al., 2020).

Figure 3. Barriers to physical activity. Self-created image.
🏢 Unfavorable Urban Infrastructure:
In many cities, urbanization has reduced safe spaces for physical activity (parks, bike lanes, recreational areas), or they are nonexistent.
Dependence on cars and public transportation has decreased incidental physical activity (such as walking to work or school).
⚠️ Barriers in Low-Income Communities:
The lack of affordable and accessible gyms can limit exercise options.
In unsafe areas, security concerns act as a barrier to activities like running or cycling.
🏫 Impact on Children and Adolescents:
The reduction of physical education in schools and increased screen time have contributed to childhood sedentary behavior.
Physical activity during childhood is crucial in preventing obesity in adulthood.
💡 Key Insight: Creating environments that encourage physical activity should be a public health priority. This includes developing safe spaces and promoting accessible programs for the entire population.
🚨 The Impact of Stigma on Health
In addition to biological and environmental challenges, people with obesity face discrimination and prejudice, significantly impacting their well-being (Sánchez-Carracedo, 2022).
Obesity stigma can lead to serious consequences, such as:
Increased risk of depression and anxiety 😔 due to constant social pressure and discrimination.
Avoidance of healthcare services 🏥 for fear of being judged, leading to delayed diagnoses and essential treatments.
Increased stress, which in turn contributes to hormonal imbalances and weight gain 🔄.
Far from being a simple aesthetic issue, obesity stigma becomes a barrier to health and well-being, discouraging many people from seeking help or receiving adequate care.
📢 A Call for a Change in Perspective
To combat stigma, it is essential to:
✔ Raise awareness among society and healthcare professionals about the complexity of obesity.
✔ Promote a science-based approach, rather than blaming individuals for their weight.
✔ Create more inclusive environments, where access to healthy food and spaces for physical activity is facilitated.
Obesity is not simply a matter of individual discipline but the result of multiple biological, social, and environmental factors. Breaking stigma is a key step in improving the quality of life of affected individuals and building a fairer and healthier society.
💙 Final Reflection: Obesity Is Not Just a Matter of Personal Choice
It is crucial to understand that obesity is not the result of a single cause but multiple interacting factors. Not everyone has the same opportunities to maintain a healthy lifestyle, and obesity stigma can worsen the situation by making access to adequate treatments more difficult.
Instead of blaming individuals for their weight, we must focus on creating an environment that promotes health and ensuring that everyone has access to nutritious food, opportunities for physical activity, and unbiased medical support.
Obesity is not a personal failure but a public health challenge that requires a science-based and empathetic approach.
Reference
Chiurazzi, M., Cozzolino, M., Orsini, R. C., Di Maro, M., Di Minno, M. N. D., & Colantuoni, A. (2020). Impact of genetic variations and epigenetic mechanisms on the risk of obesity. International Journal of Molecular Sciences, 21(23), 9035. https://doi.org/10.3390/ijms21239035
Nutter, S., Eggerichs, L. A., Nagpal, T. S., Ramos Salas, X., Chin Chea, C., Saiful, S., Ralston, J., Barata-Cavalcanti, O., Batz, C., Baur, L. A., Birney, S., Bryant, S., Buse, K., Cardel, M. I., Chugh, A., Cuevas, A., Farmer, M., Ibrahim, A., Kataria, I., Kotz, C., ... Wilding, J. (2023). Changing the global obesity narrative to recognize and reduce weight stigma: A position statement from the World Obesity Federation. Obesity Reviews, 25, e13642. https://doi.org/10.1111/obr.13642
Rubino, F., Puhl, R. M., Cummings, D. E., Eckel, R. H., Ryan, D. H., Mechanick, J. I., Nadglowski, J., Ramos Salas, X., Schauer, P. R., Twenefour, D., Apovian, C. M., Aronne, L. J., Batterham, R. L., Berthoud, H.-R., Boza, C., Busetto, L., Dicker, D., De Groot, M., Eisenberg, D., ... Dixon, J. B. (2025). Joint international consensus statement for ending stigma of obesity. The Lancet Diabetes & Endocrinology, 13(2), 485–497. https://doi.org/10.1016/S2213-8587(25)00004-X
Sánchez-Carracedo, D. (2022). Obesity stigma and its impact on health: A narrative review. Endocrinología, Diabetes y Nutrición, 69(9), 868–877. https://doi.org/10.1016/j.endien.2021.12.007
Wang, H., Dai, X., Wu, J., Wu, X., & Nie, X. (2019). Influence of urban green open space on residents’ physical activity in China. BMC Public Health, 19, 1093. https://doi.org/10.1186/s12889-019-7416-7
Ready to Get Started?
I'm here to answer any questions and help you take the first step toward better health.
Contact me
Fill out the form to request information or book your personalized nutrition consultation.

